This post may contain affiliate links, and I may earn compensation when you click on the links at no additional cost to you.
Introduction
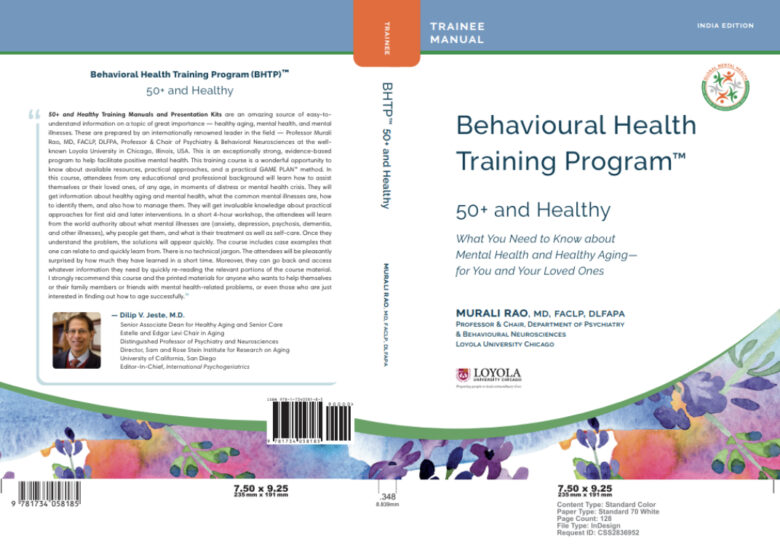
50+ and Healthy: What You Need to Know About Mental Health and Healthy Aging – for You and Your Loved Ones, was written in 2020 by Murali Rao, MD. The book outlines what seniors should know about healthy aging and how it has an effect on their mental health. It is now available as a Training Program with Trainer and Trainee Manuals, as shown above. Behavioral health and cognitive health also refer to mental health. Mark Twain once said:
Age is an issue of mind over matter. If you don’t mind, it doesn’t matter.
Why This Book Matters to Seniors
Seniors 50 and over were raised at a time when people did not seek treatment for mental illness. By age 50, seniors showing signs of mental illness lived with the triple stigma of physical disability, mental illness and ageism.
We are unable to control genetics and choices our parents made for us when we were young. But we can choose to make healthy choices while we are young. The sooner people make lifestyle changes, the easier it is to maintain good mental health by age 50.
This book is meant to help elders, Dr. Rao noted. However, people of all ages can benefit from the information in the book. Helping a person who has a mental illness “does not always require medical training, but it does require some knowledge and a mindset of openness.”
What You Need to Know: Facts About Mental Health and Mental Illness
Statistics on Mental Health
The World Health Organization (WHO) was quoted in 2001 as stating that:
One in four people in the world will be affected by mental or neurological disorders at some point in their lives. Around 450 million people currently suffer from such conditions, placing mental disorders among the leading causes of ill-health and disability worldwide.
Why Seniors Are Reluctant to Seek Help
Treatment for mental health disorders is available, according to WHO. However, almost 2/3 of people who have a known mental health disorder never seek help from a health care professional. Stigma, discrimination, and neglect are the three reasons seniors are reluctant to seek care for mental health disorders. Dr. Rao quoted WHO as saying:
Where there is neglect, there is little or no understanding. Where there is no understanding, there is neglect.
How Does Mental Health Affect Seniors?
- “350 million worldwide are believed to suffer from major chronic depression in any given year of measure.
- An estimated 44 million people worldwide are afflicted with dementia, including Alzheimer’s Disease in 2015, with some saying that the number could triple by 2050.
- The total worldwide cost of dementia is US$818 billion in 2015, growing to over $1 trillion by 2018″.
What Alzheimer’s Is… And Is Not
Alzheimer’s is not a normal part of aging. Neither is depression nor dementia. Seniors 50 and over find it easy to ask for help when they show symptom of diabetes, cancer, or heart disease. However, they are reluctant to seek help when they can no longer remember things or have a shorter attention span. Seniors 50 and older will say to themselves “I’m having a senior moment here” when they find they cannot remember things like they used to. Elders also tend to think to themselves “I didn’t used to be this slow at_______” when they refer to a mental process.
An Example of Stigma in Seniors – Dementia
Dementia carries a particularly strong stigma in American society. It includes several disorders that affect the ability to think and remember things. Alzheimer’s is most dominant with 60% of dementia cases. External stigma as it relates to dementia is “rejection and fear of the person with the disorder and of his symptoms and new and unpredictable behaviors”. A senior with dementia feels mentally confused. In addition, they are ashamed of having the disease and being unable to control its symptoms. Seniors eventually become afraid of being alone and dependent on others the rest of their lives. Stigma is confronted through education and information.
The Double Stigma of Mental Illness and Aging
The APA reminds us that “mental health conditions are treatable”; a physician can diagnose and treat them like a physical illness. Mental health disorders are nothing to be ashamed of. The person who has it should never feel ashamed because they are depressed or anxious. Neither should their family, friends, therapists, and caregivers.
What is Stigma?
Stigma is a “preconceived notion that the mental illness of any individual is dangerous to others”. Tt is easier to seek help for a physical ailment than for mental disorders. Medical professionals are not always trained to treat seniors who show signs of depression or Alzheimer’s. Some medical professionals don’t prioritize mental health as part of a person’s holistic health which includes mind, body, and spirit, Dr. Rao noted. He also emphasized there is a difference between internal and external stigma. No one would ever be criticized for having a broken arm. However, people of all ages are “beat up” for being diagnosed with a mental, emotional, or physical illness, Dr. Rao emphasized.
Stigma “around any form of mental illness should not be one of the challenges anyone has to deal with”, Dr. Rao pointed out. Seniors 50 and over should never experience stigma because they show symptoms of mental disorders.
Internal Stigma
Dementia is an example of internal stigma. Seniors show signs of internal stigma when they are reluctant to seek knowledge about their condition. They are kept from “seeking and following through with professional treatment and getting the support that is available either in the community at large or from the mental health community”. A senior is told by their family negative things about themselves. Examples include that they are “faking it”, just trying to get attention, or are too lazy or unmotivated to go out in the community. Eventually, seniors believe what society at large tells them about themselves and begin to believe it is their fault.
Losing Their Independence
By age 50, seniors begin to fear they will lose their independence and privacy. As a result, seniors fear they will no longer be able to get around on their own nor take care of themselves. They begin to fear they will now become a burden on their families and loved ones, eventually feeling abandoned. Seniors who have been independent throughout their lives may begin to feel they are a prisoner of their own mental capacity. Once seniors begin to show signs of dementia, depression or losing their hearing or sight, they begin to feel they can no longer live on their own. They are now watched 24/7 by family, friends, and health professionals.
Institutions That Stigmatize Mental Illness
Dr. Rao pointed out that the stigma of mental illness also persists in institutions, including:
- “governments.
- large and small health insurance companies.
- workplace health plans.
- workplace owners and managers.”
Mental health coverage is not always “authorized”, Dr. Rao found. As a result, a senior seeking mental health care can find it hard to get the help they need if it is not authorized by their physician.
External Stigma
Whenever there is a mass shooting, eventually it is reported that the shooter had mental health issues. But treatment was never pursued because of the stigma associated with mental illness. So, instead of seeking help for mental health issues, they shoot other people until they are killed or arrested. The shooter is generally not given an option to address his problems if he is arrested; and often remains in denial about it. In American society, a person with mental health disorders is considered dangerous to himself and others, Dr. Rao wrote.
Mental disorders include “schizophrenia, bipolar disorder, alcoholism and drug dependency”. However, these disorders are misunderstood by the public. In addition, bulimia, anorexia and substance abuse disorders are believed to be the person’s own fault and that they inwardly want to have these disorders, Dr. Rao found.
Behaviors Toward People with Mental Health Disorders
Some of the behaviors people with mental health disorders experience from others include:
- “expressions/attitudes of mistrust.
- pity or shaming/guilt-tripping.
- showing fear or dislike.
- avoiding or rejecting the individual.
- assumptions that the individual with the illness is now very dangerous and one must stay clear of them.
- that the individual is faking ii”
Why It is Hard for Seniors to Get Treatment for Mental Illness
There is a persistent belief that people suffering with mental illness are considered unapproachable, hard to talk to, hard to reason with (particularly when asked to seek medical care) and refuse to get treatment, Dr. Rao wrote. As a result, seniors who have lived with the stigma of mental illness all their lives will be reluctant to get the care they need as they age; if seniors show signs of both physical disabilities and mental health disorders, it can be even harder to get help. Historically, seniors have been made to feel ashamed of themselves and not worth any kind of care simply because they have a mental disorder. These beliefs are false.
How The Stigma of Mental Illness Can Be Stopped
Seniors with mental illness “struggle doubly hard: first with the illness and disability itself, then with the attached stigma”, Dr. Rao wrote. The only way the stigma of mental illness that be stopped is by educating family, medical professionals, and society as a whole about what mental illness is and is not. Educating the public is essential in helping seniors’ ability to live life to the fullest, regardless of their physical and/or mental health. Mental illness is only part of who a person is; it is not part of who they are holistically. Seniors should be supported instead of feared when they seek help for any physical, mental, or emotional disorder.
Facts About Mental Health and Mental Illness
What is Mental Health?
The World Health Organization (WHO) defines mental illness as:
a state of wellbeing in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community.
Mental health is the foundation of a person’s communication, emotions/feelings, learning, thinking, self-esteem/self-confidence and resilience. Mental health is the “ability to bounce back from stresses and all types of setbacks)”, Dr. Rao wrote. It is fundamental to “developing relationships and interacting socially, to personal and emotional well-being, to contributing out in the world and at home, Dr. Rao added. Mental health is the ability to be able to live in the community despite the challenges of everyday life. It is the ability to be able to think and control one’s emotions despite the problems one faces daily, to develop relationships and maintain appropriate social interaction.
What is Mental Illness?
The American Psychiatric Association (APA) defines mental illness as:
…health conditions involving changes in emotion, thinking or behavior (or a combination of these). Mental illnesses are associated with distress and/or problems functioning in social, work or family activities.
Mental illness may or may not be objective, Dr. Rao emphasized. What happens as people get older is their loved ones observe “…one or more signals or symptoms of decline or change in mental functioning, a decline or change from the prior, younger years ‘normal’.” Changes in older adults does not mean the person is suffering from mental illness, Dr. Rao said. Although mental illness is observed changes, mental, cognitive and behavioral illnesses are not the same thing, Dr. Rao found. Mental disorders “are a number of diagnosable and separately distinguishable mental, cognitive, or behavioral disorders”, just like physical disorders, Dr. Rao wrote.
What is Healthy Aging?
Aging and mental disorders such as depression and dementia are NOT a natural part of aging. Healthy “aging means good physical health and good mental health”, Dr. Rao found. Healthy cognitive and emotional aging for seniors means much more than “the absence of depression and anxiety or other disorders”. Health in this perspective means the ability to, according to Dr. Rao:
- “self-regulate/manage one’s emotions—an emotional self-control.
- the presence of contentment and happiness, natural optimism and a positive outlook.
- mastery/control over one’s behaviors.
- a sense of control over one’s world, one’s personal affairs”.
What Contributes to Mental Health in Later Life?
Like physical health, good mental health requires certain factors to remain healthy, Dr. Rao found. The data shows that these characteristics contribute to mental health, he found:
- “a high educational attainment.
- a prosperous socio-economic life.
- the habit of physical activity…
- residing in a harmonious, caring environment.
- being intellectually/socially curious and active”.
How Do These Characteristics Result in Mental/Emotional Reserves?
The characteristics named above help seniors get through the challenges they face in life. In addition,they are able to bounce back from depression and/or anxiety throughout their lives, Dr. Rao wrote. Physical strength helps the body stave off illness in later life. In contrast, the brain’s strength contributes to a person’s ability to cope with life’s stressors. Both physical and brain strength is different for each individual. A person’s emotional reserves makes a huge different whether people can resolve any challenges fairly quickly and move on from life’s challenges, Dr. Rao noted. Conversely, a lack of emotional reserves determines whether people wallow in their problems, wring their hands and stay emotional for a longer period of time, Dr. Rao found.
How Does This Work? An Example
Dementia and major depression evolve very slowly through life, Dr. Rao found. A person’s ability to self-motivate and take charge of one’s overall health is part of that person’s emotional reserve, he added. The ability to build up a person’s emotional reserves early in life “goes a long way in maintaining one’s physical, emotional and mental health”. If a person tended to be troubled over every challenge when they were younger, they will continue to have trouble coping with challenges later in life. A person’s emotional reserves, or lack thereof, is a factor in their ability to self-monitor, Dr. Rao noted. However, when people recognize emotional issues that are “mild” or “sporadic” early in life, it can help people “nip in the bud” severe emotional disorders later in life, Dr. Rao points out.
The Difference Between Positive and Negative
The power of remaining positive despite life’s stressors cannot be emphasized enough. Being positive affects a person’s ability to cope with stressors as they grow older. But we all know people who have a positive outlook on life despite tragedy. Likewise, we also know people who have a negative outlook on life over relatively minor things.
Characteristics of a Positive Individual
These are the characteristics of a positive person, Dr. Rao pointed out.
- “enthusiastic support for others’ endeavors.
- expressions of happiness and joy with one’s life.
- the ability to make lemonade out of lemons definitely represents a positive outlook”.
Characteristics of a Person Who Is Negative
Negativity arises in the following forms, Dr. Rao shared:
- “expressed or suppressed anger, fear, sadness.
- constant complaining or rude gossiping.
- jealously of others’ accomplishments.
- a doomsday outlook for one’s future.
- a ‘what’s the use’ outlook”.
Whether one is positive, or negative is the result of a person’s environment, family life, and whether or not they receive support from family, friends, educators, employers, and/or the community at large.
How Do Emotions Create/Support Physical Health or Illness?
Physical, mental and emotional health go hand-in-hand. It ultimately determines whether people will develop physical and/or mental illness by the time they turn 50. Emotions influence our physical, emotional, spiritual, social and mental/cognitive health in the following ways, Dr. Rao pointed out:
- “feelings such as chronic anger or hostility can increase coronary heart disease risk factors.
- anxiety disorder has been associated with greater physical disability and diminished well-being.
- depression is connected to a lesser health and lower quality of life, and a greater risk for death from suicide or medical illness”.
How Is Cognition Measured in the Elderly?
Characteristics of mental cognition include retentive memory, language functions such as finding words, ability to problem solve, mental processing speed, ability to pay attention and focus on a variety of things and planning and ability to make rapid decisions, Dr. Rao found. Measuring cognition in the elderly is a challenge, he acknowledged. Arthritis, certain medications, metabolic conditions and early-stage undiagnosed chronic diseases “can all impact cognition to greater or lesser degrees”, Dr. Rao emphasized.
Identifying and Understanding the Illnesses
Everyone will experience mental illness during their lifetime. As mentioned earlier, mental disorders are no different than physical disorders. However, seniors are more likely to seek treatment for physical illnesses than mental disorders. As a result, the stigma of mental illness continues to this day. It is necessary for seniors and their loved ones to become informed and educated about mental illness, Dr. Rau recommended.
The Forms of Mental Illness That Affect Seniors
Eleven forms of mental illness that affect seniors are identified and defined. However, the mental disorders that generally affect seniors over 50 will be outlined here. These mental disorders may be “exacerbated or brought on earlier in life by the presence of a specific physical disease, by poor overall physical health”, Dr. Rao noted. Alcoholism or drug abuse can make mental illness worse, adding that addiction to drugs or alcohol “affect mental, emotional, and physical health in different ways”, Dr. Rao wrote. These mental disorders affect different people in different ways, Dr. Rao stressed.
Depression & Bipolar Disorder
Major Depressive Disorder
Depression or major depressive disorder is a mood disorder that can disturb a person’s daily activities, work routine and relationships.
Symptoms of Depression
- “lack of interest or pleasure in activities that used to provide enjoyment.
- lack of mental attention/focus.
- difficulties sleeping”.
- lose interest in food and start to lose weight.
- start to gain weight due to overeating.
Loved ones should be concerned if the above symptoms affect the senior’s daily activities and interactions with others longer than two weeks
Bipolar Disorder
Bipolar disorder is characterized by an individual’s extreme mood swings that are polar opposites. A person diagnosed with bipolar disorder will initially show signs of depression, followed by manic behaviors.
Manic mood swings are characterized by a “euphoric or high-energy mood, combined by over-confidence or extremes in other emotions such as anger”. In addition, seniors in the manic stage may also be extremely talkative, feel they can get by with less sleep, and take risks that are unthinkable in their depressed state.
Possible Causes
There is no specific cause to bipolar disorder. However, there are biological, psychological, and environmental causes for major depression and bipolar disorder, Dr. Rao noted, including:
- genetic factors;
- general chronic health issues including Parkinson’s disease, diabetes, vascular disease, arthritis and cancer;
- personality factors including being overly sensitive and being easily angered;
- how an individual deals with stressors or an inability to deal with stressful situations.
Treatments
Treatment for depression and bipolar disorder include a combination of self-treatment, changes in lifestyle initiated by the patient, and treatments facilitated by mental health professionals, Dr. Rao said. Other suggested treatments include lifestyle changes including aerobics or stretching exercises such as tai chi. Journaling and music therapy is also helpful. Cognitive behavioral therapy (CBT), therapy focusing on problem-solving, family therapy, prescription of anti-depressant medications following an assessment, and “a structured life review with a therapist” are also helpful, Dr. Rao added.
Anxiety
Anxiety affects everyone regardless of age. However, it generally “has its roots and early appearance in younger years”, Dr. Rao said. Anxiety is defined as “feelings of fear, anxiousness or nervousness, irritation/irritability, impatience or feeling on edge, anger, worry, stress”. It must be – anxiety is not part of aging. It is possible that it possibly began when the person was younger. If anxiety was not addressed and treated by their 50s, it continued into their “golden years”. Anxiety varies from mild worrying to a panic attack that has the potential to paralyze mind and body.
Signs and Symptoms
- Presenting itself through racing thoughts in which the mind either races with nervousness or worry or is empty as in a panic attack,
- Behaviors including obsessive/compulsive disorders (OCD),
- Situations resulting in visible distress or completely avoiding a situation,
- “Inability to sleep peacefully, resorting to/increasing use of alcohol or other detrimental substances”,
- Physical symptoms of anxiety including sweaty palms, racing heartbeat, shaking, dry mouth, upset stomach or muscular aches.
Causes
- “Social phobia, where being with people causes anxiety,
- Agoraphobia or fear of crowded or tight places”,
- Panic disorder, in which paralyzing or extreme anxiety is for a shorter period of time; it may appear to be inappropriate or unprovoked at a given time, but it also occurs without warning,
- Post-traumatic stress disorder (PTSD), caused by a violent and frightening event including experiences in war, being involved in a violent accident or being physically assaulted.
Additional Causes
Additional causes of anxiety include traumas suffered during childhood, poverty background, fear of being unable to pay the bills or find a job, having a sensitive personality, or being raised to believe that the world is a threatening place, Dr. Rao noted. An individual may also feel unstable and begin to believe they are unable to take care of themselves or even survive in the world. Anxiety that is constant or prolonged eventually leads to suicidal thoughts and behaviors.
Treatments
The treatments outlined earlier by Dr. Rao for depression and bipolar disorder can also be used for anxiety.
Mental Confusion and Dementia
Dementia affects a person’s ability to make decisions, think or remember things that delays the ability to do everyday activities, Dr. Rao points out. It “is a progressive decline in cognitive abilities, which translates to reduced memory recall, ability to plan or carry out a task with focus, language disability”, Dr. Rao noted. In addition, “Alzheimer’s disease is the most common type of dementia”.
Part of the stigma behind Alzheimer’s disease is that it has been jokingly referred to as “Old Timer’s Disease”. It must be emphasized again that dementia and Alzheimer’s is not a normal part of aging.
Mental Confusion and Mental Illness
Mental confusion as it relates to mental health is characterized as
…. a poor alertness or attention capability, disorientation as to one’s surroundings or in relation to time, unclear or illogical speech and/or inability to track a conversation…disconnection with current reality, impaired memory as regards more recent events, etc.
Signs/Symptoms of Mental Confusion/Dementia
- Memory loss, characterized by forgetting things more often than previous years.
- “Misplacing items or placing them in inappropriate places.
- Difficulty finding one’s words or completing sentences.
- Becoming lost while driving or walking.
- Mood swings”.
Additional Symptoms of Mental Confusion and Dementia
Another symptom of dementia is decreased analytical judgment, Dr. Rao pointed out. As a result, decline of analytical judgment for seniors 50 and over progresses over several years, occurs in any combination and begins very slightly, Dr. Rao pointed out. Consequently, because dementia develops slowly throughout a person’s life, it is most often associated with seniors 50 and over, Dr. Rao added.
Causes
Other diseases eventually lead to dementia, Dr. Rao found. In addition, while Alzheimer’s is the most common primary disease leading to dementia, it is caused by several factors. For example, vascular cognitive impairment, also called vascular dementia, “often goes hand-in-hand with Alzheimer’s disease”, Dr. Rao wrote. In addition, Alzheimer’s may be caused by a major stroke, several smaller strokes or any “disease affecting blood vessels in the brain”, Dr. Rao added. Genetic factors such as brain injury may lead to dementia later in life.
Additional Physical Conditions Leading to Dementia
- high blood pressure/hypertension,
- type 2 diabetes,
- obesity,
- smoking.
Treatment
Lifestyle and dietary changes can help prevent the onset of dementia; Dr. Rao suggested. As a result, the earlier in life these changes are implemented the better, Dr. Rao recommended.
Lifestyle Changes that Can Delay the Onset of Dementia
- Diet – animal products should be reduced because of unhealthy unsaturated and trans fats; however, eating plant-based foods should be increased.
- Supplements – vitamin E or B12, and multi vitamins should be guided by a physician, while herbal supplements such as gingko biloba are also helpful.
- Aerobic exercise – swimming, cycling or brisk walking is recommended 3-5 times per week.
- Cognitive stimulation – lifelong and continuous learning including word games and puzzles.
- Psychological intervention – when a senior’s behavior becomes difficult, it is recommended that a mental health professional help family members identify triggers and work on strategies together to manage them.
Substance Abuse Disorders
Patients suffering from substance abuse have a history of co-existing anxiety disorders such as post-traumatic stress disorder (PTSD) or panic disorder, Dr. Rao found. In addition, substance abuse disorders are more likely to co-occur with mental disorders such as depression and bipolar disorder, Dr. Rao found.
Most Common Forms of Substance Abuse
The most common forms of substance abuse include cannabis abuse, or addiction to cigarettes or tobacco. Hard street drugs and prescribed opioids or pharmaceutical drugs are other forms of substance abuse. Prescription drugs are more dangerous and easily accessible than street drugs. Seniors who are prescribed several drugs for various ailments may easily get them mixed up, with deadly consequences. Younger people who become addicted to opioids steal them from their parents’ or grandparents’ medicine cabinets.
Suicide
Suicide is the “harshest indicator of the presence of mental distress”. While people of all ages are affected by suicide, it is most difficult when a senior takes his/her own life when they feel they’re unable to cope with the pressures of life. Seniors tend to deny they are depressed. Or they become ashamed to admit to family and/or mental health professionals that they are suffering from mental health disorder. Seniors eventually came to believe there is no alternative to live with their behavioral health disorder(s) except to end their lives.
Statistics on Mental Health and Suicide
Dr. Rao offered statistics on indicators of mental illness in the United States in 2017 including:
- “Drug overdoses took 70,000 American lives.
- 7% of the American adult population suffered at least one major depressive episode”.
While the above statistics “may not be a dependable precursor to suicide or suicidal thoughts, it is a strong indicator of mental illness and mental distress in our population”, Dr. Rao noted. He also found that firearms that have become more of a common concern in seniors’ neighborhoods, are used in “half of all suicides”.
Why Suicide, Substance Abuse and Anxiety Are Considered Mental Health Issues
People are stunned to hear that suicide ideation, substance abuse and anxiety disorders are considered behavioral health issues, Dr. Rao found. There are certain “life circumstances” or stressors from the outside that merge with an individual’s internal stress levels, including:
Environmental
A major stressor is financial, in which there is an absence of savings. Subsequently, there is less available income that can be unreliable. As a result, people 50 and over are concerned about the rising cost of medical and preventative health care on an already limited budget.
Technology
Technology comes with great expectations for young and old users alike. Seniors 50 and older believe that everyone is following along with the latest trends and are on social media daily. Consequently, they also believe that “everyone is ‘digitally connected’ to everyone else”.
A negative influence of social media for seniors is that everyone’s life is better than their own. As a result, seniors believe their lives are worse than everyone else’s. This is a double-edged sword. For example, seniors believe they are not as adept at social media as their younger relatives. As a result, seniors feel depressed because their lives are not as happy and fulfilling as everyone else’s supposedly is. However, we need to remember is that people put the best parts of their lives on social media. They don’t include doctor visits, disagreements with family members, etc.
Outside or Social Factors
Seniors are concerned about safety and security in their neighborhoods. They are particularly concerned about “the need for transportation to access any products or services”. For example, seniors become anxious and worried about their ability, or lack of ability, to maintain access to access medical care and groceries.
Internal Stressors
Examples of internal stressors include thoughts of “I’m not keeping up”, “I can’t do it alone”, and “I’m so lonely”. Internal stressors include feelings of anxiety, depression, grief, fear, rage/outrage and anger. These feelings are often not addressed for fear of being stigmatized. Consequently, these “emotions entwine with negative outcomes in the health and wellness of the body, in a spiraling cycling effect”. If these feelings are not dealt with, they can eventually lead to physical and mental illness.
Case Studies
Dr. Rao presents six case studies as follows:
- Health as a Holistic Achievement
- Physical Decline and Loss of Independence
- Food
- Taking Care of the Home
- Loss of Income and Insurance Coverage
- Depression Therapy
The elder’s case, including his/her history, is presented. The circumstances of the senior’s history are included. In some cases, the intervention of medical health professionals and the ultimate outcome are also included. In addition, the person’s accident that led to the need for intervention is included. Their mental health treatment plan and biggest risk in not seeking treatment are also included.
Encouragement For Seniors Suffering from Depression
Dr. Rao quoted a man who sought treatment for depression. He was asked what advice he could give someone who knew someone suffering from depression. This was his response:
They can’t help themselves. They don’t have the energy or the motivation to do so. And probably not the information, either. Take him gently by the arm, make the appointment, go with him to it, get him started, and just keep on loving him.
Practical Approaches for First Aid and Later Interventions
People have free will. Consequently, they can choose to make the right choices about lifestyle and getting help. Genetics is only 1/3 of developing mental illness as you age but taking necessary steps to make the right choices to prevent physical and mental illness is 2/3. With the assistance of family and medical professionals, seniors can control depression, anxiety and other mental health disorders as they get older.
National Alliance on Mental Illness
Founded in 1979, the National Alliance of Mental Illness (NAMI), is a valuable resource. Consequently, NAMI can help a senior and their loved ones take steps to help them become well in mind and body. Education, support, advocacy, and public awareness are the tools used to enable seniors live a normal and happy life. Families should follow suggestions from NAMI on the following Dos and Don’ts, Dr Rao suggested.
Do’s and Don’ts
Do’s
- “First Do No Harm”
- Choose a quiet time with few to no interruptions or distractions
- Use the correct medical terminology provided by the person’s doctor or therapist
- Give them the opportunity to talk and respond to you, taking your time
- Show respect and understanding for how they explain and understand their symptoms
- Always give the person hope for recovery by always offering encouragement to see a professional or continue therapy.
Don’ts
- Never be confrontational, judgmental or “sound or look exasperated” remembering it’s “not about you or your stresses”.
- Show hostility
- Act patronizing or condescending to them. Be mindful it’s not about you or your opinion that their condition isn’t serious
- Tell them to “just pray” and things will change for them
- Get upset at their distress
- Talk at them, but instead “carry on a quiet, calm two-way conversation…”
Myths and Realities About Mental Health
- Myth – It’s genetic so we really can’t do anything to change it; Reality – Only 1/3 of all factors that determine or prevent mental and physical health as we age is genetic.
- Myth – I don’t have a supportive system, including family, Reality You won’t know how your family really feels if you don’t let them know what the new aging pattern is for you and what you need. In addition, it would be helpful for your family to know what you are really going through by seeking help in the community without fear of stigma.
How Seniors Can Control Their Mental Health
Seniors need to take charge of their own mental health, Dr. Rao suggested. Some of these changes include, but are not limited to:
- Social and family stigma – it is possible to change the way you think about mental illness. For example, you can choose to break the stigma by telling yourself both mental and physical decline as you age is inevitable. In addition, you can also become aware that treatment, education, and health care is available. All you need to do is find it for yourself and your loved ones.
- Exercise – “use it or lose it”. You don’t need to join a health club but do what you like., including walking in nature. Exercise improves both physical and cognitive health. It is possible exercise can lower the risk or even prevent mental illness (Dr. Rao noted that there is continuing research on this last concept).
- Go with someone to appointments -seniors should go with a relative to appointments together. “Two heads are better than one”. The family member and the senior should share symptoms and circumstances with the doctor. Comparing notes on what the doctor said and acting on it for further treatment is also helpful.
- Most important, love yourself and the senior. “Love and compassion are powerful healers”.
Making a GAME Plan for Helping Others in Distress
Transitioning is not easy for anyone at any age. Seniors want to remain in their homes as long as possible. They would prefer to move out only when they or their families believe they can no longer safe living there due to declining mental and physical health. The senior and their family should focus on moving the senior from autonomy to adaptability, Dr. Rao suggested. It takes an entire family and the senior to adapt to adjusting to a “new normal”. When a senior moves from independence and autonomy to dependence, it “means that the individual counts more on his strengths than on his (new) weaknesses”, Dr. Rao noted.
Steps of the GAME PLAN
GAME
G -Growth – Help seniors thrive in an environment that is mentally healthy. Opportunities to learn, grow and have new experiences are available at any age.
A – Awareness – Be aware of the signs/symptoms for identifying a mental health crisis or issue. For example, it is helpful for the senior if a loved one notices if their elderly relative either doesn’t recognize his//her need or is unable to express it.
M – Match the senior with the best available medical, financial, transportation, or home support needs.
E – Enquire – Follow-up should include making sure the senior’s needs are met short-term; however, it should be satisfactory for seniors and their loved ones. All adjustments should be made if the senior’s needs are assessed incorrectly.
PLAN
P – Prepare for the senior’s prolonged accommodations or needs that evolve over a period of time.
L – Life/work balance – Never over-extend a family member caring for a loved one. Subsequently, resources should be provided as needed. A senior’s self-care should enable them to remain self-sufficient and independent.
A – Assess – Initial assessments may change over time. However, it is helpful for the senior and their family to check on their progress for any new needs.
N – Network – Help the senior maintain their social and medical/home support networks. No one can do it alone. This includes the family member with the best intentions.
Myths and Realities about Mental Illness
- Myth – There’s nothing wrong with you. It’s all in your head. Just make a decision ot be well and snap out of it. Reality – If a senior is experiencing something that appears to be “off”, then there is something wrong. Seniors should consult their primary doctor. The doctor can refer them to the appropriate mental health professional.
- Myth – Cognition and particularly memory naturally declines with age. Reality – Not all seniors experience “cognitive or memory decline”.
- Myth – Since seniors consider themselves healthy as a rule, they don’t need to be concerned with “that type of illness either”. Reality – “One in four Americans will deal with depression each and every year”.
- Myth –The belief “Once you have contracted a mental illness, it’s all over...” makes seniors believe they will never recover from mental illness; Reality – People diagnosed with mental illness do recover completely with the right treatment. “Recovery” means they have gone through the appropriate treatment and healing process. Therefore, they are able “live, work, study and fully participate in life as they wish to”.
Triggers
Seniors may have “strong coping mechanisms they can call on”; However, triggers need extra attention. Examples of triggers include:
- Alcohol, tobacco and/or substance abuse.
- Losing a spouse after years of marriage.
- Terminal illness of a senior or a loved one.
- Physical disability.
- Illnesses of a physical nature resulting in changes in memory, emotions, and thoughts.
- Change in environment. For example, moving to either an assisted living facility or a child’s home. In addition, feeling abandoned by family when the last child moves out of the home.
Your Own Healthy Aging
You are lucky if are in your 40s, 50s or 60s and have always been in good health, Dr. Rao points out. However, you cannot become content you will always be in good health.
Humans are “creatures of habit”. We have lived 70% (or more) of life “on routine changes and behaviors, routine thoughts and emotions”, Dr. Rao noted.
The Body as a Holistic Organism
The following areas represent a whole and balanced approach to well-being, Dr. Rao noted:
- “Physical health
- Mental health
- Spiritual health
- Social heath
- Emotional health”
Physical diseases eventually kill the body. However, mental disorders “‘kill the ability or desire to live a full and satisfying life”. In addition, as the body suffers, so does the brain and mind. The holistic nature of our beings that help us maintain good physical and mental health cannot be denied.
We Are What We Eat and Think
Earing too much salt and sugar creates an imbalance in our systems, Dr. Rao found. In addition, tobacco, alcohol and “street drugs” affect our brains with toxic chemicals. Prescription drugs are more dangerous than “street drugs”. As a result, medical professionals are paying more attention to drugs and other substances that can result in destruction of the body holistically.
A senior’s outlook on life makes all the difference on healing when they become ill. Negative emotions can “both create and perpetrate physical illnesses”, Dr. Rao cautioned.
Other Habits That Support Holistic Health
Healthy aging is the result of healthy habits. Seniors who develop habits early in life that don’t include medication or therapy can prevent mental illness later in life, Dr. Rao found. Healthy aging is a result of preventative and non-medical solutions begun at a young age, Dr. Rao mentioned, including:
- Getting exercise in a safe environment for seniors.
- Keeping the brain/intellect active.
- Strong spirituality.
A senior should consider themselves lucky if their doctor doesn’t prescribe drugs, Dr. Rao noted. However, all drugs have side effects. As a result, seniors should take prescriptions as directed, Dr. Rao recommended.
For more information on mental health and healthy aging, click the link to the book at the beginning of this article.
Conclusion
Dr Rao writes at the conclusion of this book:
We are holistic beings. Not just a body. Not just a mind. Our physical, emotional, mental, and behavioral aspects entwine, entangle, and combine in ways unique to each of us. Knowledge, acted upon, is your personal power to heal and be healthy.
About the Author
From the NNDC India Foundation (National Network of Depression Centers):
Dr. Murali Rao is the Professor and Chairman of the Department of Psychiatry and Behavioral Neurosciences at Loyola University Medical Center in Chicago. He specializes in liaison and emergency psychiatry. Additionally, he serves as a member of multiple professional bodies including the American College of Psychiatrists, the Academy of Psychosomatic Medicine, CINP, the Indian Psychiatric Society, and the American College of forensic Psychiatry.
Dr. Rao has received multiple awards and fellowships including Distinguished Life Fellow by the APA, Outstanding Academician Award by the Indo-American Psychiatric Association, and the Master Teacher Award by the Stritch School of Medicine. Dr. Rao has also had more than 50 journal publications.